Shoulder Stabilisation Surgery
What is Shoulder Stabilisation Surgery?
Shoulder stabilisation surgery aims to reduce or eliminate abnormal shoulder joint motion, which can result in pain, weakness, or dislocation.
The surgery involves repairing or reconstructing the torn or stretched ligaments that hold the shoulder joint in place.
This stabilises the shoulder joint and prevents it from dislocating or partially dislocating.
Who is Suitable for Shoulder Stabilisation Surgery?
Shoulder stabilisation surgery is typically recommended for patients who have experienced shoulder dislocation or subluxation. This can occur due to a traumatic injury or repetitive strain over time, such as in the case of athletes who play overhead sports like tennis. Patients with persistent shoulder instability may be suitable for shoulder stabilisation surgery if conservative treatment, such as physiotherapy, fails to resolve their symptoms.
What are the Benefits of Shoulder Stabilisation Surgery?
Shoulder stabilisation surgery offers numerous benefits to patients, including:
- Reduced risk of shoulder dislocation: After surgery, the shoulder joint is stabilised, reducing the risk of dislocation or subluxation.
- Pain relief: Surgery can help alleviate pain caused by shoulder instability and other shoulder injuries.
Type of Shoulder Stabilisation Surgery Options
- Shoulder Labral Repair Surgery
- Remplissage procedure
- Latarjet Stabilisation Surgery
Shoulder Labral Repair Surgery
Shoulder reconstruction is required for patients with shoulder instability to improve stability, restore function and prevent recurrent shoulder joint dislocations.
With the excessive movement of the ball on the socket, the shoulder may dislocate.
Shoulder dislocation can be partial or complete.
- A partial dislocation occurs when the ball of the upper arm comes partially out of the socket. It is referred to as a subluxation.
- A complete dislocation occurs when the ball comes out of the socket.
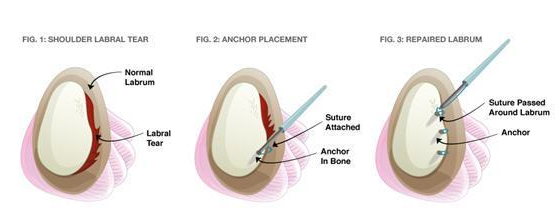
Shoulder instability most commonly occurs due to a Bankart injury or tear. Bankart tear is a specific injury to a part of the shoulder joint called the labrum. The labrum is a ring of fibrous cartilage that surrounds the glenoid and stabilises the shoulder joint.

Bankart tears can lead to recurrent dislocations, feelings of looseness, lack of strength and pain or clicking. Shoulder instability may be caused by injury, falling on an outstretched hand, or repetitive overhead sports such as basketball, volleyball or weight lifting.
Patients with shoulder instability may have severe pain, swelling, popping or grinding sound, partial or complete dislocation, loss of sensation or partial paralysis and loss of function.
If conservative treatments such as immobilisation, analgesic medicines, physiotherapy and activity modification fail to relieve the shoulder instability, your surgeon may recommend reconstruction surgery.
Remplissage Procedure
The Remplissage procedure treats shoulder instability associated with a Hill-Sachs lesion. This procedure is typically performed with labral repair.
During a dislocation, the back resulting in a divet is called a Hill-Sachs lesion. The Remplissage procedure is designed to address this issue by filling the defect in the humeral head with soft tissue, which can help stabilise the joint and prevent further dislocations.
In the Remplissage procedure, the fracture surface is freshened, and anchors with sutures are used to tie the adjacent rotator cuff tendon into the defect, filling the defect. The portion of the humeral head where the defect is filled is excluded from the joint and can no longer slip over the front of the socket, thus preventing dislocation.


Latarjet Stabilisation Surgery
Latarjet stabilisation surgery is a surgical procedure primarily used to treat recurrent shoulder dislocations or instability in patients with significant bone loss in the shoulder joint. The procedure is named after the French surgeon Michel Latarjet, who described it in 1954.
The main goal of Latarjet stabilisation surgery is to restore the stability and function of the shoulder joint. It addresses two key factors: bone loss and soft tissue laxity.
During the procedure, the surgeon removes a small piece of bone, called the coracoid process, along with the attached tendons from the scapula (shoulder blade). This bone graft is then transferred to the front of the shoulder joint and fixed to the anterior (front) part of the glenoid (the shallow socket of the shoulder joint). This adds bone to the deficient area, increasing the joint's stability.
Additionally, the attached tendons help create a "sling effect" that further stabilises the shoulder joint during movement. Combining the bone graft and the sling effect helps prevent future dislocations and provides better stability for the shoulder joint.
What to do Before a Shoulder Stabilisation Surgery?
There are several things patients can do to prepare for surgery. These include:
- Quit smoking: Smoking can delay healing and increase the risk of complications during and after surgery. It's best to quit smoking several weeks before surgery.
- Stop taking certain medications: Certain medications, such as blood thinners and nonsteroidal anti-inflammatory drugs (NSAIDs), can increase the risk of bleeding during surgery. The surgeon may recommend stopping taking these medications before surgery.
- Get in shape: Physical fitness can help improve surgical outcomes and speed up recovery time. Try to get in the best physical shape possible before surgery.
- Make arrangements for aftercare: Patients may need help with everyday tasks after surgery, such as getting dressed or preparing meals. They should arrange for a family member or friend to assist during recovery.
What Happens During Shoulder Stabilisation Surgery?
Several surgical techniques can be used for shoulder stabilisation, such as arthroscopic Bankart repair, open Bankart repair, and Latarjet procedures. The specific procedure chosen depends on the patient's condition, bone loss or other structural issues, and the surgeon's preference.
These are the general steps involved in an arthroscopic shoulder stabilisation surgery, which is a less invasive approach compared to open surgeries like the Latarjet procedure:
- Anaesthesia: The patient is given general anaesthesia, which puts them to sleep during the procedure. Sometimes, a regional nerve block is administered to relieve pain during and after the surgery.
- Positioning: The patient is positioned in a way that allows the surgeon to access the shoulder joint easily. This is typically done with the patient lying on their side or in a semi-seated position (also known as a "beach chair").
- Arthroscopy: The surgeon makes small incisions (portals) around the shoulder joint to insert the arthroscopic instruments. An arthroscope, a small camera mounted on a thin tube, is inserted through one of the portals, allowing the surgeon to visualise the inside of the joint on a monitor.
- Assessment: The surgeon assesses the extent of the damage, the condition of the labrum (the cartilage rim around the glenoid), and the ligaments and tendons surrounding the joint.
- Repair: The surgeon will reattach the labrum to the glenoid using small anchors and sutures.
- Closure: After the repair, the surgeon removes the arthroscopic instruments and closes the incisions using sutures or skin adhesives.
What to Expect After the Surgery?
After surgery, the patient is moved to a recovery room and closely monitored as the anaesthesia wears off. Once the patient is awake and stable, they can usually go home on the same day. It is important to realise that a Bankart repair is not a quick fix, as it can take 10-12 weeks for the tissues to heal normally. The repair has to be protected from any weight-bearing forces until it is healed, usually 12-16 weeks. You MUST follow instructions strictly, as only the surgeon knows the ligaments' state during the repair. If you try to speed up the rehab for whatever reason, you risk tearing the repair.
Shoulder Stabilisation Surgery Recovery Plan
Recovering from shoulder stabilisation surgery can be a lengthy process that requires patience and commitment. The following is a general recovery plan that patients can expect to follow:
- Immediately after surgery: You'll wake up with a sling around your shoulder to immobilise the joint and prevent movement. Depending on your surgeon's instructions, you must wear the sling for several weeks.
- Post-operative rehabilitation: Your surgeon will provide you with specific exercises to perform to help restore the range of motion and strength in your shoulder. Physiotherapy will be an integral part of your treatment and recovery.
- Returning to normal activities: Returning to normal activities can take several months to return to normal activities after shoulder stabilisation surgery. You may need to avoid certain activities, such as sports that involve overhead movements or heavy lifting, for up to a year after surgery.
- Follow-up appointments: You'll need to attend regular follow-up appointments with your surgeon and physiotherapist to monitor your progress and ensure that your shoulder is healing properly.
Shoulder Stabilisation Surgery Prognosis
The prognosis for shoulder stabilisation surgery is generally good, with most patients experiencing significant improvements in shoulder function after surgery. However, the success of the surgery depends on several factors, including the extent of the injury, the type of surgery performed, and the patient's commitment to the recovery process. Patients who follow their surgeon's and physiotherapist’s instructions for post-operative rehabilitation are more likely to experience positive outcomes.
Shoulder Stabilisation Surgery Risks
As with any surgical procedure, shoulder stabilisation surgery carries certain risks and potential complications. These include:
- Infection: There is a risk of infection at the surgical site, which may require additional treatment.
- Bleeding: Excessive bleeding can occur during or after surgery, requiring additional medical attention.
- Nerve or blood vessel damage: The nerves or blood vessels surrounding the shoulder joint may be damaged during surgery, resulting in numbness, weakness, or other complications.
- Shoulder stiffness: Some patients may experience stiffness in the shoulder joint after surgery, requiring additional physical therapy.
- Recurrence of shoulder instability: In a minority of cases, the repaired or reconstructed ligaments may fail to hold the shoulder joint in place, resulting in a recurrence of shoulder instability.
What if Shoulder Stabilisation Surgery is Delayed?
If shoulder stabilisation surgery is delayed, it's important to take steps to manage the symptoms of shoulder instability in the meantime. These will include physiotherapy or lifestyle changes to reduce the risk of dislocation or subluxation. However, delaying surgery may increase the risk of further damage to the shoulder joint, making the surgery more complex or less effective.
If you're experiencing recurrent shoulder instability, it's best to consult with an orthopaedic surgeon to determine the best course of action for your specific situation.
Selangor Specialist Suites,
Nambour Selangor Private Hospital,
62 Netherton Street,
Nambour, QLD, 4560
All Rights Reserved | Dr Tendai Mwaturura