Shoulder Joint Replacement
What is Shoulder Joint Replacement?
Shoulder joint replacement, also known as shoulder arthroplasty, is a surgical procedure that involves replacing the shoulder's damaged or diseased ball-and-socket joint with an artificial joint.
The procedure is performed under general anaesthesia and involves removing the damaged bone and cartilage and replacing them with a metal or plastic prosthesis.
Who is Suitable for Shoulder Joint Replacement?
This procedure is usually recommended for patients who experience severe shoulder pain and limited mobility due to osteoarthritis or other degenerative conditions, such as rheumatoid arthritis or post-traumatic arthritis.
Other conditions requiring shoulder joint replacement include rotator cuff tears, avascular necrosis, or severe shoulder fractures.
To be considered for shoulder joint replacement, patients must undergo a thorough evaluation by an orthopaedic surgeon.
What are the Benefits of Shoulder Joint Replacement?
The benefits of shoulder joint replacement include improved shoulder function, reduced pain, and an increased range of motion.
After the surgery, patients can expect to experience less pain, improved strength, and better shoulder range of motion, which can greatly improve their quality of life.
In addition, shoulder joint replacement can help patients return to their normal daily activities, such as work, hobbies, and sports.
Types of Shoulder Joint Replacement
Your surgeon will carefully evaluate your situation before choosing the right Shoulder Joint Replacement.
There are different types of Shoulder Joint Replacement Surgery:
- Anatomical Total Shoulder Replacement
- Reverse Total Shoulder Replacement
- Stemmed Hemiarthroplasty
- Resurfacing Hemiarthroplasty
Anatomical Total Shoulder Replacement
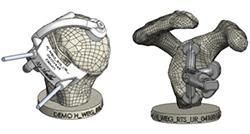
Typically, the total shoulder joint replacement surgery involves replacing the arthritic joint surfaces with a highly polished metal ball attached to a stem and a plastic socket.
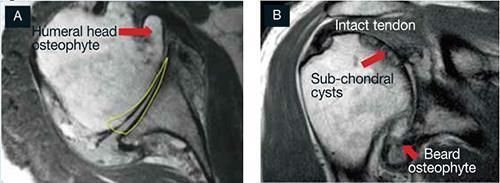
Patients with bone-on-bone osteoarthritis and intact rotator cuff tendons are good candidates for conventional total shoulder replacement.
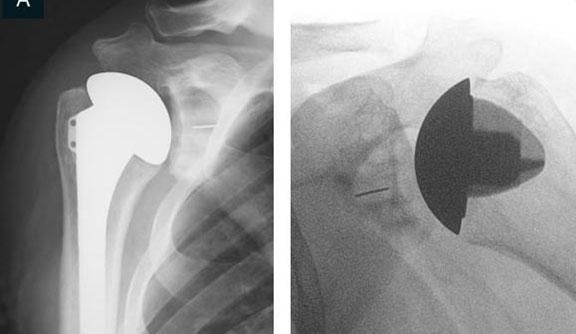
Reverse Total Shoulder Replacement
For patients suffering from a completely torn rotator cuff, severe arthritis with rotator cuff tearing, or a failed anatomic shoulder joint replacement, a conventional total shoulder replacement may result in ongoing pain and limited mobility. A reverse total shoulder replacement is indicated in such situations.
In reverse total shoulder replacement, the socket and ball are switched. A metal ball is attached to the shoulder blade, and a plastic socket is attached to the upper arm bone. This allows the patient to use the deltoid muscle to lift the arm even though the rotator cuff tendons are torn.

Stemmed Hemiarthroplasty
Depending on the patient's shoulder condition, the surgeon may replace only the head of the humerus bone (ball). This procedure is called hemiarthroplasty.
Typically, the head of the humerus is replaced with a metal ball and stem, similar to the component used in a total replacement.

Resurfacing Hemiarthroplasty
With arthritis of the shoulder, this offers an alternative to the standard stemmed replacement.
Resurfacing Hemiarthroplasty involves replacing the joint surface of the humeral head with a cap-like prosthesis without a stem.
This is a popular option for patients who are young or very active, as it avoids the risk of component wear and loosening that can occur in the other procedure.

Before Shoulder Joint Replacement
Before undergoing shoulder joint replacement, patients must undergo a thorough evaluation by an orthopaedic surgeon. The surgeon will review your medical history, physical condition, and imaging studies to determine if you are a suitable candidate for the procedure.
Diagnostic methods include:
- Taking a medical history emphasising pain, disability and general health.
- Performing a physical examination of a range of motion and muscle strength.
- Arranging imaging (x-rays and scans) to understand the type of arthritis, the integrity of the rotator cuff and bone loss.
Shoulder Imaging
- X-rays - These images help to determine the extent of damage in your shoulder. They can show loss of the normal joint space between bones, flattening or irregularity in the shape of the bone, bone spurs and the ball riding high on the socket after chronic tendon tears.



- MRI - can create detailed images of both hard and soft tissues. An MRI can produce cross-sectional images of internal structures required if the diagnosis is unclear. It is the most accurate way of determining associated rotator cuff tears or muscle wasting.
- CT scans - are most accurate at detailing bone wear and can be used to create 3D models for surgical planning and implant placement

- Ultrasound - can be a useful screen to check the integrity of the rotator cuff tendons.
Surgery Preparation
In preparation for shoulder joint replacement, patients should follow these guidelines:
- Quit smoking: Smoking can interfere with healing and increase the risk of complications.
- Lose weight: Excess weight can stress the shoulder joint, making it more difficult to recover from surgery.
- Inform your surgeon about any medications: Some medications, such as blood thinners, may need to be discontinued before surgery.
- Prepare your home: Patients should make necessary modifications to their home, such as installing handrails, to ensure a safe and comfortable recovery.
Shoulder Joint Replacement Surgery
The procedure is performed under general anaesthesia and typically takes two to three hours. The steps involved in a shoulder joint replacement include:
- Incision: The surgeon makes an incision in the front of the shoulder to expose the damaged joint.
- Removal of damaged bone and cartilage: The surgeon removes the damaged bone and cartilage from the shoulder joint, leaving a clean surface for the prosthesis.
- Preparation of bone surfaces: The surgeon prepares the remaining bone surfaces for the prosthesis by smoothing them and shaping them to fit the prosthesis.
- Placement of the prosthesis: The prosthesis is inserted into the prepared bone surfaces of the shoulder joint. The prosthesis may be made of metal, plastic, or ceramic.
- Closure of incision: The surgeon closes the incision with sutures or staples and applies a dressing to the shoulder.
After the Surgery
After undergoing shoulder joint replacement, patients typically spend one night in the hospital. During this time, they will be monitored for any signs of complications. The surgeon will prescribe pain medication to manage discomfort, and physical therapy will begin within the first few days after surgery.
Shoulder Joint Replacement Recovery Plan
Physiotherapy is essential to the recovery plan. Patients will work with a physiotherapist to perform exercises and stretches that will help improve shoulder range of motion and strength. The physiotherapist will also guide how to perform daily activities, such as dressing and grooming while protecting the shoulder joint.
Patients must wear a sling for several weeks after surgery to protect the shoulder. They should avoid lifting heavy objects or engaging in strenuous activity for at least six weeks after surgery. Full recovery may take several months to a year, depending on the patient's age, health, and lifestyle.
Shoulder Joint Replacement Risks
As with any surgical procedure, shoulder joint replacement carries some risks. Potential complications include:
- Infection
- Blood clots
- Nerve damage
- Dislocation of the artificial joint
- Loosening or wearing of the artificial joint
- Allergic reaction to the prosthesis
Patients should discuss potential risks and benefits of shoulder joint replacement with their surgeon before undergoing the procedure.
Shoulder Joint Replacement Prognosis
The prognosis for shoulder joint replacement is generally good. Most patients experience significant pain relief and improved shoulder function after the surgery. However, the long-term success of shoulder joint replacement depends on factors such as age, overall health, and lifestyle. Patients who are overweight or engage in high-impact activities may experience more wear and tear on the artificial joint, which can lead to premature failure.
What if Shoulder Joint Replacement is Delayed?
If shoulder joint replacement is delayed, patients may experience continued pain and shoulder stiffness, significantly impacting their quality of life. Delayed treatment may also increase the risk of complications and require more extensive surgery.
Selangor Specialist Suites,
Nambour Selangor Private Hospital,
62 Netherton Street,
Nambour, QLD, 4560
All Rights Reserved | Dr Tendai Mwaturura